A number of different types of medications are currently in use to treat glaucoma. If your doctor feels you will benefit from treatment with medication, she will work with you to find one that is appropriate for you. Your doctor may prescribe one medication or a combination of two or more medications to provide the most effective treatment for you. At times, finding the right medication for you can be a trial and error process since you may not respond to or may have side effects to some of the medications.
All glaucoma medicines have the possibility of having side effects, some of which can be uncomfortable. A few side effects can be quite serious, but those are not common. Please let your doctor know of any side effects you are experiencing from the medication. It is possible to experience these side effects either initially or over a long period of time. Your doctor will work with you to find a medication that is the most comfortable for you.
Over time, the medications you are using may start to lose their effectiveness or the glaucoma can progress without your knowledge. For this reason, it is important to have regular check ups so adjustments to your treatment can be made by your physician before your condition worsens. Adjustments may include changing the drop you are using or using a different combination of drops that may be more effective in controlling the pressure in your eye.
Remember, you and your doctor must work together to determine the best medicines for you. Never change or stop taking your medications without consulting your glaucoma physician.
The following is a list of different types of glaucoma medications and their possible side effects:
Additional information:
Prostaglandin Analogues are drugs that work to lower pressure in the eye by improving fluid drainage. These drops are powerful and require use only once per day. As with most medicines, however, some people will be non-responders.
Possible side effects. A rare side effect may be a darkening of eye color or eyelid. Often, there is an increased growth of eyelashes. Side effects can also include redness, itching, burning and blurred vision.
| Medicine | Brand Name | Image |
| bimaprost | Lumigan | view image |
| latanaprost | Xalatan | view image |
| travaprost | Travatan-Z | view image |
Beta-blockers decrease pressure inside the eye by reducing the amount of aqueous fluid your eye makes. They are most effective when used in the morning. It is prudent to check with your primary care doctor before starting drops in this class, particularly if you have certain medical conditions. People with asthma, some kinds of heart disease or low blood pressure should be very careful about using beta-blockers to treat their glaucoma. Also, if a patient is on other "blocker" medicines for other health problems, the combined effect of the drugs could cause problems.
Possible side effects include possible respiratory problems, lowered heart rate and blood pressure, blurred vision, tiredness, forgetfulness, and changes in blood cholesterol levels.
| Medicine | Brand Name | Image |
| timilol hemihydrate 0.50% | Betimol | view image |
| timilol maleate 0.5% | Istalol | view image |
| timilol maleate 0.5% | Timoptic | view image |
| timilol maleate (gel) | Timoptic XE | view image |
Alpha-Adrenergic Agonists are eye drops that lessen the amount of aqueous fluid the eye makes and may also increase flow of fluid out of the eye. These drops are sometimes used after laser surgery to prevent sudden rises in pressure.
Possible side effects include allergic reactions, dry mouth, burning of the eyes, dilated pupils, nasal decongestion and drowsiness.
| Medicine | Brand Name | Image |
| apraclonidine | lopidine | |
| brimonidine tatrate | Alphagan, Alphagan-P | view image |
Carbonic anhydrase inhibitors come in pills or drops. They reduce the amount of aqueous fluid the eye makes. The pills have a higher level of side effects than do the drops. The pills may be used when other attempts to control the glaucoma have not worked fully. The eye drop form of these medications has less severe side effects and is quite powerful.
Possible side effects. The more common eye drop form of this drug may cause stinging, burning, a feeling of something in the eye, and an odd taste in the mouth. Taken as pills (only rarely nowadays), these drugs can have side effects throughout the body, including fatigue, tingling in the hands and feet, depression, frequent urination, anemia, kidney stones, loss of appetite, weight loss, diarrhea, and stomach cramps. Monitoring the dose of the oral pill and taking the medicine with food may help. Pregnant women and people sensitive to sulfa-related drugs should take these medicines with caution if at all. A toxic reaction may occur if taken with large doses of aspirin. Very rarely, these drugs can lead to serious conditions known as Stevens-Johnson syndrome and aplastic anemia.
| Medicine | Brand Name | Image |
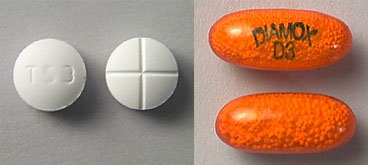
| acetazolamide (pill) | Diamox | view image |
| brinzolamide (drop) | Azopt | view image |
| dorzolamide (drop) | Trusopt | view image |
| methazolamide (pill) | Neptazane |
Combinations containing two medicines in the same bottle:
| Medicine | Brand Name | Image |
| dorzolamide/timolol maleate | Cosopt | view image |
Follow your treatment plan
It's up to you to follow your treatment plan and have regular follow-up visits. These visits are usually scheduled every 3 months with testing. At follow-up visits, your doctor will check to see if your glaucoma is getting worse. Remember to report anything you believe may be a side effect of the medicine you are taking.
Don't skip doses!
Take your medicine as scheduled. Skipping doses of your medicine may put your vision in danger and mislead your doctor. Be sure to tell your doctor if you've missed any doses.
With a chronic disease like glaucoma, it can be hard to remember to use medicines as directed. It may help to link taking medicine to the things you do every day like eating meals or brushing your teeth.
After evaluating your progress, your doctor may try changing your doses, switching medicines or changing other parts of your treatment to find the best results for you. Sometimes simple changes like adjusting your schedule to take your medicines at mealtimes or before bed can make your drug routine more comfortable.
Prescription eye drops for glaucoma help maintain the pressure in your eye at a healthy level and are an important part of the treatment routine for many people. Always check with your doctor if you are having difficulty.
Remember:
Steps for putting in eye drops:
If you are still having trouble putting eye drops in, here are some tips that may help.
If your hands are shaking: Try approaching your eye from the side so you can rest your hand on your face to help steady your hand.
If shaky hands are still a problem, you might try using a 1 or 2 pound wrist weight (you can get these at any sporting goods store). The extra weight around the wrist of the hand you're using can decrease mild shaking.
If you are having trouble getting the drop into your eye: Try this. With your head turned to the side or lying on your side, close your eyes. Place a drop in the inner corner of your eyelid (the side closest to the bridge of your nose). By opening your eyes slowly, the drop should fall right into your eye.
If you are still not sure the drop actually got in your eye, put in another drop. The eyelids can hold only about one drop, so any excess will just run out of the eye. It is better to have excess run out than to not have enough medication in your eye.
Having trouble holding onto the bottle? If the eye drop bottle feels too small to hold (in cases where a dropper isn't used and the drop comes directly from the bottle), try wrapping something (like a paper towel) around the bottle.
You can use anything that will make the bottle wider. This may be helpful in some mild cases of arthritis in the hands.
Assistive devices are available to help you put in your eye drops.